Southeast Health Plans, Inc. is a company that provides health plan administrative services to self-insured employers. The company focuses on employers with 50 to 500 employees. Many of these employers already have HMO, PPO, or major national insurance carrier health plans. However, the major national insurance companies often overlook our target market. While over 80% of companies with 500 or more employees are self-insured, only about 25% of Atlanta area companies with 50 to 500 employees have self-insured plans.
The market for self-insured and administrative services includes companies that are currently self-insured and companies that have other types of health plans and might consider shifting to self-insurance. Quality administrative and consultative services play a role in the shift to self-insurance. Southeast Health Plans, Inc. is led by experienced management and has formed a strategic alliance with Blair Mill Administrator, a subsidiary of Blue Cross/Blue Shield of Pennsylvania, to provide benefits management services.
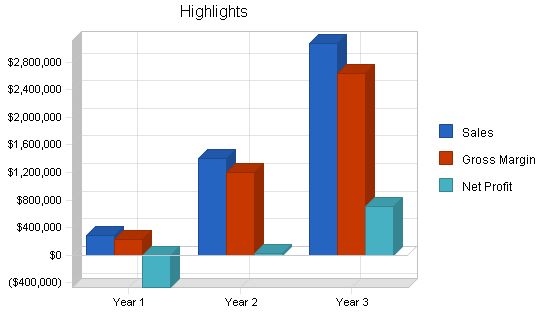
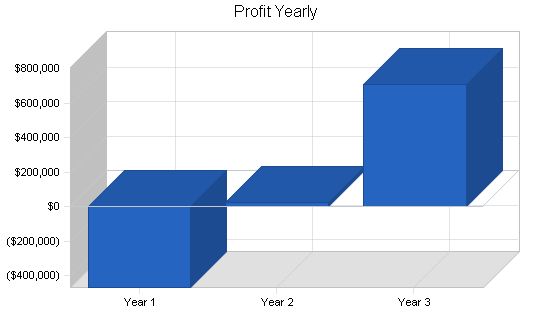
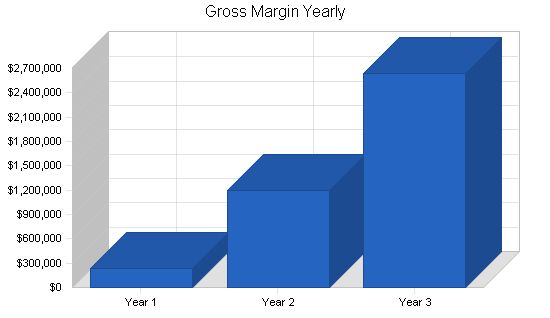
In five years, Southeast Health Plans, Inc. aims to generate over $5 million in revenue and achieve a net profit after tax of $1.6 million. The company expects to become profitable in year three with after-tax earnings of $560 thousand. As a marketing organization and service provider, the company will have high margins, with gross margins of over 80% (excluding sales incentive costs) and approaching 50% after all operating expenses, once market penetration has reached maturity.
The key to success for Southeast Plans, Inc. is to secure initial capital to effectively market its services in the metro Atlanta area and northern Georgia. Adequate professional sales staffing is crucial. Once successful, the company will expand throughout Southeastern markets while controlling costs, particularly with sales and marketing programs, to ensure expansion is funded by internal cash flow.
Contents
1.1 Objectives
The company’s objectives are:
- To initiate co-operative marketing with media in the Atlanta metro market.
- To hire and train sales staff to implement a sales lead follow-up strategy.
- To have 4,800 employees under management by the end of year one.
- To approach break-even by the end of year two and increase market share.
- To shift to earnings in year three and accelerate gross margin contributions.
- To expand regionally with both media and sales personnel to penetrate new markets and consolidate service capability.
- To achieve cost benefit through an expanding provider network without compromising patient care.
- To have more than 98,000 employees under management by the end of year five.
1.2 Mission
Southeast Health Plans, Inc. provides small and mid-size employers with a comprehensive benefits administration program that controls health benefits costs while providing access to quality health care. By combining self-insurance, stop-loss programs, and efficient plan administration, Southeast delivers quality care and freedom of choice at a fair price.
1.3 Keys to Success
The keys to success in this business are:
-
Marketing: Southeast Health Plans will sell directly to employers and through independent insurance brokers and agents. It is essential to establish name recognition and maintain closing ratios of at least 5% of leads per year.
Company Summary
Southeast Health Plans, Inc. is a service company founded by experienced medical insurance industry executives to serve and capitalize on the growing number of small and midsize companies seeking to control health benefits costs and manage risk through self-insurance.
Southeast utilizes Blair Mill’s existing services, products, and infrastructure to provide necessary service without establishing proprietary programs. Blair Mill’s provider networks serve employers with multiple locations or a wide-spread workforce.
Southeast targets employers with 50 to 500 employees and offers all-encompassing benefit management programs. Services include managed care, patient care management, provider networks, administrative services, flexible plan design, underwriting and actuarial services, comprehensive information management, data reporting, and stop-loss insurance administration.
2.1 Start-up Summary
The following tables and chart summarize the start-up requirements and anticipated funding.
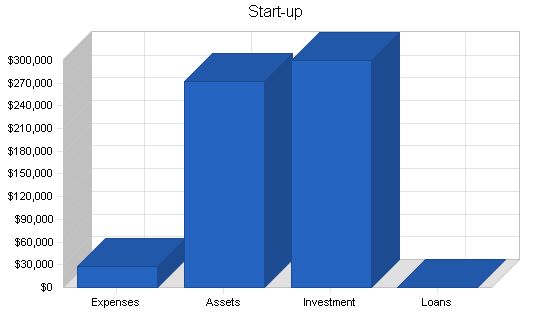
Start-up
Requirements
Start-up Expenses
Legal
$0
Consultants
$12,500
Offering Expenses
$15,000
Total Start-up Expenses
$27,500
Start-up Assets
Cash Required
$272,500
Other Current Assets
$0
Long-term Assets
$0
Total Assets
$272,500
Total Requirements
$300,000
Start-up Funding
Start-up Expenses to Fund
$27,500
Start-up Assets to Fund
$272,500
Total Funding Required
$300,000
Assets
Non-cash Assets from Start-up
$0
Cash Requirements from Start-up
$272,500
Additional Cash Raised
$0
Cash Balance on Starting Date
$272,500
Total Assets
$272,500
Liabilities and Capital
Liabilities
Current Borrowing
$0
Long-term Liabilities
$0
Accounts Payable (Outstanding Bills)
$0
Other Current Liabilities (interest-free)
$0
Total Liabilities
$0
Capital
Planned Investment
Private Placement ’96
$300,000
Investor
$0
Additional Investment Requirement
$0
Total Planned Investment
$300,000
Loss at Start-up (Start-up Expenses)
($27,500)
Total Capital
$272,500
Total Capital and Liabilities
$272,500
Total Funding
$300,000
2.2 Company Ownership
Southeast Health Plans, Inc. is a privately-held Georgia corporation. It is owned by its founders and managing partners: James J. Peters, Thomas R. Cormier, and L. Richard Schumacher, MD.
The company has been established with the founders’ own capital. The founders have negotiated an exclusive strategic alliance with Blair Mill Administrators for certain markets in the state of Georgia.
The founders are now seeking to extend outside ownership interest to raise the funds required for business expansion.
2.3 Company Locations and Facilities
Southeast Health Plans, Inc. currently occupies office space in Atlanta, GA.
The phone number is … and the fax number is … .
The current offices provide sufficient space to launch business in the Atlanta and north Georgia market. More space will be required as the Atlanta market matures and central services are provided to other geographic markets. Additionally, local sales offices will be required in other markets.
Increases in rental costs are included in the plan’s pro forma profit and loss.
Services
Health care in the United States has changed rapidly over the past two decades. Large insurance companies and private physicians have been replaced by HMOs, Managed Care Plans, and TPAs. A TPA, like Blair Mill, administers health care functions for a company that would have been handled by an insurance company. Businesses now demand more in terms of service and analysis than traditional support institutions have been providing. Claims processing alone does not help a business analyze and control its health benefits plan or control costs. Southeast has compiled a service mix that includes Network Administration Services, Network Contracting Services, Policy Formation and Quality Assurance, and Marketing Services.
Health benefits are a fact of life for any business. The small and mid-size business is concerned with cost control and administration. A full array of TPA self-insured services includes claims experience analysis and cost projections, plan design consulting, comprehensive plan analysis, provider network analysis, plan documentation, stop-loss brokerage and administration, prescription drug programs, vision benefits administration, dental benefits administration, COBRA administration, short-term disability administration, worker’s compensation services, and custom tailored services.
3.1 Competitive Comparison
Health plans for businesses and their employees are a highly competitive multi-billion dollar industry. Well-known national insurance companies and HMOs seek the employer’s dollar. Southeast Health Plans believes there is a niche that is too small for large national companies to cover and not well-served by other TPAs. By providing quality services at a fair price, Southeast aims to gain a competitive advantage in the market.
3.2 Sales Literature
Sales materials and literature prepared by Blair Mill will be utilized by Southeast. Advertising executions and direct mail pieces are being developed. A professional presentation to prospective clients is provided through a Blair Mill portfolio and video tape.
3.3 Fulfillment
The strategic alliance with Blair Mill Administrators provides the principal source of health plan administrative services for Southeast. Southeast earns revenue from enrollment sales and cost advantages in the delivery of health care services. This relationship reduces the risk associated with an early stage health services provider.
3.4 Future Services
Future services will include establishing a geographic network of clients and health care providers throughout the southeast. As Southeast Health Plans grows, it will begin to look less like a TPA and more like a Health Plan. Options exist to finance the shift to a Health Plan company, including mezzanine or venture funding and potential IPO or acquisition.
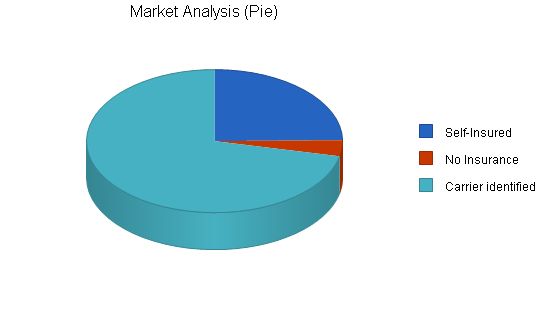
Potential Customers Growth Year 1 Year 2 Year 3 Year 4 Year 5 CAGR
Self-Insured 10% 446 491 540 594 653 10.00%
No Insurance 0% 66 66 66 66 66 0.00%
Carrier identified 0% 1,289 1,289 1,289 1,289 1,289 0.00%
Total 2.76% 1,801 1,846 1,895 1,949 2,008 2.76%
4.2 Service Business Analysis
Together the national insurance carriers, HMOs, and PPOs account for 72% of the current market for employer-based health plan services. The majority of HMOs and PPOs have their own marketing and sales programs which include company employed sales forces. National insurance companies may have company sales people or may utilize independent insurance agents. Both have strong media programs.
Neither, however, provide the mix of services that Southeast Health Plans can provide. Nor can they provide the quality/cost ratio or the ancillary consultative and custom services of Southeast combined with Blair Mill. Southeast feels that this entire employer universe of 1,801 companies is vulnerable to penetration.
4.2.1 Competition and Buying Patterns
Buying patterns vary by the size of the employer and according to his internal organization.
The company with 50 to 100 employers may have health care handled by the owner or a key executive. Often it is the responsibility of the Personnel Administrator as an individual (if that function is internal to the company). Also, Personnel Administration may be outsourced, but benefits may not. Sometimes an independent benefits brokerage firm handles all recommendations.
Larger companies from 200 to 500 employees may have Personnel Departments of several people. They might also employ a broker or a consultant.
Thus, it is imperative that Southeast have flexible programs and sales and marketing efforts that are targeted to a diverse set of potential buying patterns.
Customer buying patterns for health plan coverage tend to revolve around annual renewal dates. That’s when competition intensifies from traditional providers. Southeast will have a significant marketing advantage since an employer may retain Southeast for its proprietary service mix at any time. Southeast can initiate service for a client by helping him analyze and administer his current plan. Often, such an engagement will progress to full service and to administration of self-insurance.
4.2.2 Business Participants
Insurance carriers provide economic protection only. Such protection is at a high cost. Deductibles are increasing and the employer’s ability to handle the cost burden of medical insurance coverage is diminishing. Compromises must be made in the extent of coverage, the size of the deductible, the medical services included, or often the employee is required to cover an increasing percentage of the cost of his own plan as a payroll deduction. These are all unattractive options for both the employer and the individual client. The spiraling cost of health care is the culprit.
HMOs have gained substantial market share over the past two decades, exceeding the national commercial insurance carriers by a wide margin. However, these plans have been ruled primarily by cost containment strictures. Freedom of choice is limited – there is a perception that the quality of care is at an all-time low. Liability issues are beginning to surface based on compromised or neglected care due to cost parameters. Many service costs are not adequately covered under these plans and the provider base of physicians is extremely dissatisfied with compensation allowances. Many physicians complain that the freedom of decision is diminishing constantly from time and cost constraints imposed upon them. The ultimate client, the individual patient, is equally dissatisfied. Thus, the employer becomes dissatisfied as well.
The market niche for the quality TPA is ripe for picking. However, services must be of high quality. Many small TPAs promise high levels of service but often don’t deliver as promised because of the expense of building the internal resources required to compete effectively. Southeast Health Plans, by virtue of its alliance with Blair Mill Administrators, already has the necessary resources in place.
4.2.3 Distributing a Service
HMOs and Managed Care Companies are experienced and effective direct marketers. They employ media marketing and company sales forces to good effect. The primary problem they face is increasing dissatisfaction with their product. They will not be able to provide the multi-regional, customizable services that an increasing number of employers will demand. In addition, self-insurance is contrary to the buy-and-resell philosophy of these providers.
Many national insurance companies market through company sales forces and independent brokers and agents. Herein lies a potential barrier to entry into the small company market for an emerging TPA. Often the company has a pre-existing relationship with an insurance agent that may encompass a broader range of insurance services than health care. The company is, in fact, buying a “package” of varied insurance coverages that are necessary to business operation and also happen to include health care coverage. The task here is one of general education about the potential of self-insurance programs. If the insurance agent doesn’t provide this alternative he stands to eventually lose the health insurance coverage. But his current “franchise” with his client can be a barrier.
It is the intention of Southeast Health Plans both to market directly and to work through independent agents to reach their existing clients. A competitive agent compensation program is in place to accomplish this objective. The company intends to both work with independent agents who recognize the mutual value of cooperation or to sell in head-to-head competition with those who don’t.
Ultimately, product, service, and price will prevail. All sales forecasts of the company recognize the time line of market penetration and have realistic market share goals.
Strategy and Implementation Summary
With provider services already in place, the launching of sales and marketing strategies and implementation is the next task of Southeast Health Plans. Executions include print media in targeted general business publications, direct mail programs, and sales contact follow-up.
In addition, contacts and seminars directed at independent agents and benefit brokerage firms will be launched. Additional sales materials will be produced that are targeted specifically toward these intermediary “customers.”
Print media utilized will be the weekly Atlanta Business Chronicle. An extensive direct mail lead generation campaign will also be employed, targeted at employers, brokers, and consultants. Both will be followed by direct sales contact by Southeast’s professional sales executives.
5.1.1 Pricing Strategy
Pricing for administrative services provided by Blair Mill is billed on a cost-per-employee basis.
Actual medical costs within self-insured programs will vary as a combination function of negotiated provider service costs coupled with the level of stop-loss (deductible) coverage.
Revenues to Southeast Health Plans, Inc. are determined by sales commission formulas and also by cost advantages for medical services negotiated by Southeast contracted care providers. Thus, if Southeast provides medical service to the plan at a cost below the expected cost for the same service, differential revenue accrues to Southeast.
In both cases, there is a time lag to realization of revenue. Sales commissions are paid 30 to 60 days in arrears based upon collection from customers. Service cost revenues are based upon actual services utilized and are also paid 30 to 60 days in arrears. All revenue projections included in this plan are based upon these delayed collection premises while all expenses are treated as cash when incurred (even if paid on 30-day terms). Thus, all cash flow analyses will err on the conservative side.
According to the terms of the existing agreement with Blair Mill, Southeast Health Plans will earn 25% of medical facility cost savings (as incurred) in years one and two and 17% in year three.
All services revenues generated by Southeast for new clients produced for Blair Mill will be paid as sales commissions according to the formula contained in the agreement. (A copy of the agreement is available to investors).
The sales commissions are as follows:
– 11.2% of all fees in the first year of the sale.
– 2% of all fees in the second and third years.
– 5% of all fees in the fourth year and in each renewal year thereafter.
– Blair Mill administrative service costs average about $15 per month per employee covered.
– In addition, commissions on new stop-loss policies will average 15% in year one.
5.2 Sales Strategy
The sales strategy for Southeast Health Plans is based upon concentrated targeted direct marketing with sales call follow-up. Closing ratios are estimated at only 5% of prospects to yield cumulative covered plan employees projected in the sales forecasts. Thus, higher closing ratios are potentially possible and would accelerate growth and revenue beyond the forecasts.
All forecasts are based upon per employee estimates. Dollar charges are based upon “A,” “B”, and “C” size markets and the prevailing costs for medical care for those markets respectively. Back-up market data is too extensive to include in this plan.
Note: An “A” market is defined as metro Atlanta. A “B” market is a population center over one million. A “C” market is any market below one million in population.
Annual projected revenues are illustrated in the chart below.
Monthly sales forecasts for the first year are included in the appendix.
Note: A total of 23 employer groups have already become active through Blair Mill as of November 1, 1996. Revenues based upon health care cost savings will show up in the beginning of 1997. Initial monthly revenues are based upon these employer groups, which represent approximately 1,500 employees (already 31% of the first year goal of 4,800 covered employees).
On an average annual basis, the revenue projections for health care savings revenue to Southeast are based upon $7.40 per employee for 1997. This number is for “A” markets. “B” markets are estimated at $5.66, and “C” markets at $3.71 per employee. Rationale: Atlanta is over-bedded and under-utilized, while in smaller markets the reverse is true.
Additional selling and retention fees are added to the above estimates to obtain total revenue numbers. In “A” markets, for example, this is set at $1.75 for new employees and at $0.75 for renewal/retention fees.
5.2.1 Sales Forecast
The following sales forecasts are based upon the premises previously presented.
Management feels these forecasts are highly attainable.
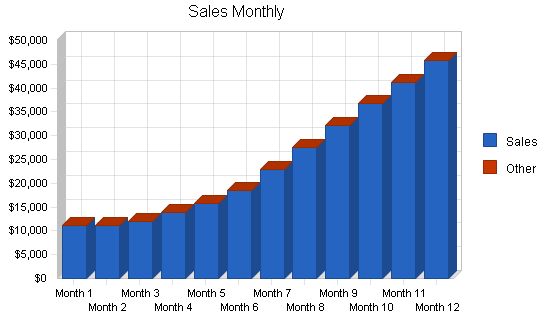
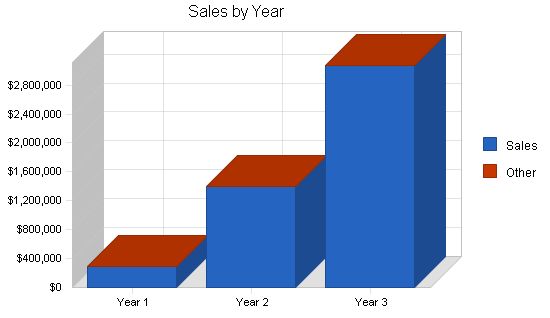
Sales Forecast
Year 1 Year 2 Year 3
Sales $288,599 $1,399,223 $3,067,966
Other $0 $0 $0
Total Sales $288,599 $1,399,223 $3,067,966
5.3 Strategic Alliances
In addition to the primary strategic alliance with Blair Mill, Southeast Health Plans, Inc. has formed alliances on the health care provider network side, providing cost advantages and guaranteed revenue through Blair Mill for billed medical services.
The initial agreement with Columbia Health Care Systems will provide coverage to a substantial portion of metro Atlanta. A second agreement is forthcoming with Independent Health Care Providers, including DeKalb Medical Center, Scottish Rite Hospitals, and Northside Hospital System, resulting in comprehensive availability for Atlanta Metro and including 52% of available hospital beds. Cost savings are reflected in revenue projections per covered employee.
5.4 Milestones
Milestones already achieved:
– Founder “seed” funding of $200K to develop and research plan, secure strategic alliances, and establish initial infrastructure.
– Strategic alliances in place with Blair Mill and with Columbia Health Systems.
– 23 employer groups and 1500 employees already under managed care contracts.
– 52% of Atlanta metro area available hospital beds under contract at acceptable cost discounts.
Milestones to be achieved:
– Obtain $300K capital to staff and launch full sales and marketing executions.
– Present Blair Mill products and services to 50 of the largest employers in our target market by March 1, 1997.
– Reach the stated first-year goal of 4800 covered plan employees by January 1, 1998.
– Reach the first-year revenue goal of $288K by December 31, 1997.
– Attain break-even cash flow by the end of year two.
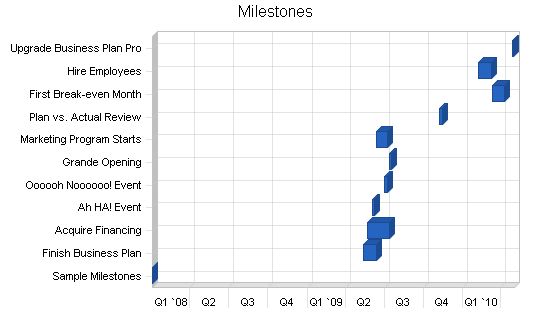
Milestones:
– Sample Milestones: 1/4/2008 – 1/4/2008, $0 Budget, ABC Manager, Department Department
– Finish Business Plan: 5/13/2009 – 6/12/2009, $100 Budget, Dude Manager, LeGrande Fromage Department
– Acquire Financing: 5/23/2009 – 7/12/2009, $200 Budget, Dudette Manager, Legumers Department
– Ah HA! Event: 6/2/2009 – 6/7/2009, $60 Budget, Marianne Manager, Bosses Department
– Oooooh Noooooo! Event: 7/2/2009 – 7/7/2009, $250 Budget, Marionette Manager, Chèvre deBlâme Department
– Grande Opening: 7/12/2009 – 7/17/2009, $500 Budget, Gloworm Manager, Nobs Department
– Marketing Program Starts: 6/12/2009 – 7/7/2009, $1,000 Budget, Glower Manager, Marketeers Department
– Plan vs. Actual Review: 11/7/2009 – 11/14/2009, $0 Budget, Galore Manager, Alles Department
– First Break-even Month: 3/11/2010 – 4/10/2010, $0 Budget, Bouys Manager, Salers Department
– Hire Employees: 2/7/2010 – 3/9/2010, $150 Budget, Gulls Manager, HRM Department
– Upgrade Business Plan Pro: 4/28/2010 – 4/30/2010, $100 Budget, Brass Manager, Bossies Department
– Totals: $2,360 Budget
Management Summary:
The founding management of Southeast Health Plans has 75+ accumulated years of industry experience. They are well versed in industry fundamentals, educated in the evolution of the health care services industry, and share a vision for the successful positioning of Southeast Health Plans, Inc.
6.1 Organizational Structure:
The three founders will manage the company’s growth jointly as managing partners. Staff, sales, and marketing personnel will report to them through a sales manager (with industry experience) who has also been identified. Future branch offices will have a general manager.
6.2 Management Team:
– James J. Peters, Managing Partner: Over 25 years experience in sales and marketing management in employee benefits, securities, and real estate.
– Thomas R. Cormier, Managing Partner: Over 25 years of experience in employee benefits, including group insurance underwriting and regional sales support.
– L. Richard Schumacher, MD, Managing Partner: Internal medicine specialist with 25 years in practice, leadership positions in managed care organizations, and experience as a respected advisor/consultant in the managed care industry.
– Jeffrey E. Farmer, Sales Manager: Sales management professional with a strong record of production achievement in employee benefits and managed care sales.
6.3 Personnel Plan:
The following table illustrates the Personnel Plan for Southeast Health Plans, Inc. Specific needs, compensation, and timing are indicated for each position. Future branch office staffing needs are lumped together as one line item.
– Total Payroll: $441,492 in Year 1, $757,000 in Year 2, $981,000 in Year 3.
6.4 Management Team Gaps:
Two gaps exist within the management team: a Chief Financial Officer (CFO) and a Business Development (Capitalization) Specialist. These functions will be performed on a consultative basis in the first year of operations. The CFO position can later be filled full-time, and capitalization will be handled by Investment Banking Relationships. The interim positions will be staffed by:
– Interim CFO: *Confidential and Proprietary information omitted.*
– Interim VP Corporate Development: Timothy Dineen, Principal and Founder of Leprechaun Capital. Experienced in raising capital for public and private companies in an advisory capacity.
6.5 Other Management Considerations:
An advisory board of prominent managed health care professionals is being assembled. These individuals are available for consultative assignments and strategic planning. The preliminary advisory board includes:
– Dr. Nancy W. Ashbach, MD, MBA: Former CEO of MetLife of Colorado and Utah, with expertise in outcomes management, reference standard benefits, and doctor/plan relationships.
– Dr. Leslie Moldauer, MD: Psychiatrist and former National Director of Mental Health and Chemical Dependency Services at MetLife Health Care Management Corporation, specializing in the integration of mental health and chemical dependency programs into health plans.
– Dr. Tighe E. Shomer, MD: Medical Director for a national managed care company, partner and director in a medical software and hardware company, advisor to Fortune 500 clients on managed care issues, particularly preventative care and quality improvement.
The financial plan for rapid, but controlled growth for Southeast Health Plans, Inc. is presented in detail in the following sections. Initial capitalization is $1 million, and the company will be debt-free (barring any interim management decisions). The company has significant IPO potential and/or acquisition opportunities in the future.
7.1 Important Assumptions:
The financial plan is based on the following assumptions:
– Current Interest Rate: 8.00%
– Long-term Interest Rate: 8.00%
– Tax Rate: 33.00%
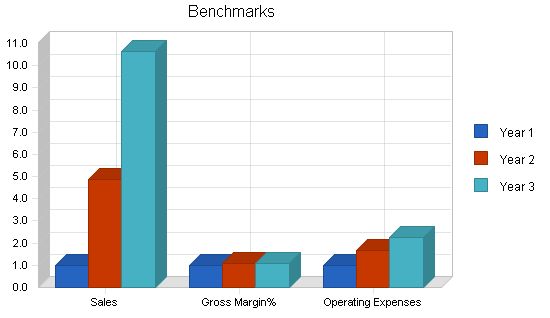
7.2 Key Financial Indicators:
Key financial indicators include increasing sales volume, maintenance and improvement of margins, and ongoing cost control.
Break-even Analysis:
Monthly break-even will be achieved before the end of year two, considering fixed initial market overheads. As cost control and market maturation occur, profitability will accelerate, with increased disproportionate gains as market development costs are offset by a critical mass of baseline business in each new market.
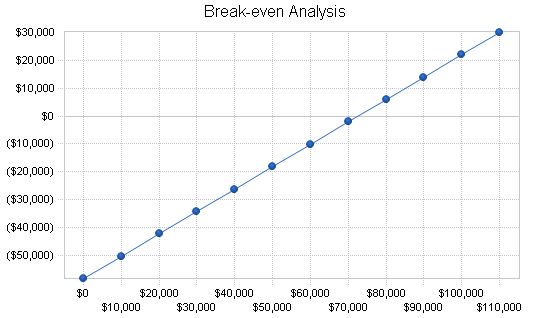
Break-even Analysis:
Monthly Revenue Break-even: $72,637.
Assumptions:
Average Percent Variable Cost: 20%.
Estimated Monthly Fixed Cost: $58,291.
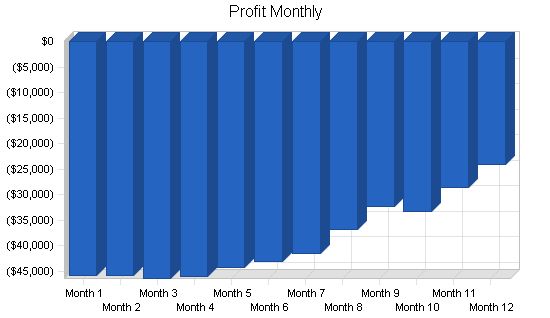
7.4 Projected Profit and Loss:
Southeast Health Plans, Inc. projects overall profitability in year three.
Pro Forma Profit and Loss
Year 1 Year 2 Year 3
Sales $288,599 $1,399,223 $3,067,966
Direct Cost of Sales $57,000 $201,000 $427,500
Other Costs of Sales $0 $0 $0
Total Cost of Sales $57,000 $201,000 $427,500
Gross Margin $231,599 $1,198,223 $2,640,466
Gross Margin % 80.25% 85.63% 86.07%
Expenses
Payroll $441,492 $757,000 $981,000
Marketing/Promotion $180,000 $288,000 $456,000
Depreciation $0 $0 $0
Rent $30,000 $90,000 $120,000
Telephone/Utilities $12,000 $24,000 $30,000
Payroll Taxes $0 $0 $0
Contract/Consultants $36,000 $0 $0
Total Operating Expenses $699,492 $1,159,000 $1,587,000
Profit Before Interest and Taxes ($467,893) $39,223 $1,053,466
EBITDA ($467,893) $39,223 $1,053,466
Interest Expense $0 $0 $0
Taxes Incurred $0 $12,944 $347,644
Net Profit ($467,893) $26,279 $705,822
Net Profit/Sales -162.13% 1.88% 23.01%
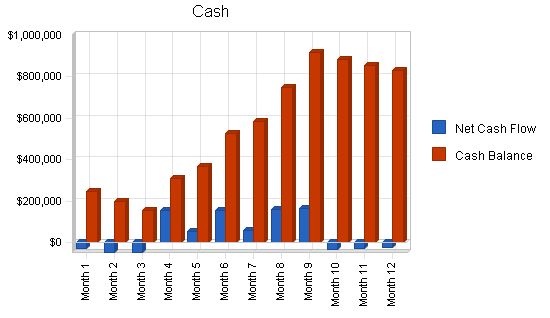
7.5 Projected Cash Flow
Cash flow is critical for business success.
Our business model includes significant margin for error and ensures that we never run out of cash. We secure initial and second round investments before they are needed to account for potential time lag in closing deals.
Future growth is based on a debt-free, internally funded model. Achieving targeted sales revenues will generate the necessary cash to execute expansion plans as presented.
In the event of future sales shortfalls, plans can be curtailed or postponed.
| Pro Forma Cash Flow | |||
| Year 1 | Year 2 | Year 3 | |
| Cash Received | |||
| Cash from Operations | |||
| Cash Sales | $288,599 | $1,399,223 | $3,067,966 |
| Subtotal Cash from Operations | $288,599 | $1,399,223 | $3,067,966 |
| Additional Cash Received | |||
| Sales Tax, VAT, HST/GST Received | $0 | $0 | $0 |
| New Current Borrowing | $0 | $0 | $0 |
| New Other Liabilities (interest-free) | $0 | $0 | $0 |
| New Long-term Liabilities | $0 | $0 | $0 |
| Sales of Other Current Assets | $0 | $0 | $0 |
| Sales of Long-term Assets | $0 | $0 | $0 |
| New Investment Received | $1,000,000 | $0 | $0 |
| Subtotal Cash Received | $1,288,599 | $1,399,223 | $3,067,966 |
| Expenditures | Year 1 | Year 2 | Year 3 |
| Expenditures from Operations | |||
| Cash Spending | $441,492 | $757,000 | $981,000 |
| Bill Payments | $286,967 | $593,351 | $1,318,251 |
| Subtotal Spent on Operations | $728,459 | $1,350,351 | $2,299,251 |
| Additional Cash Spent | |||
| Sales Tax, VAT, HST/GST Paid Out | $0 | $0 | $0 |
| Principal Repayment of Current Borrowing | $0 | $0 | $0 |
| Other Liabilities Principal Repayment | $0 | $0 | $0 |
| Long-term Liabilities Principal Repayment | $0 | $0 | $0 |
| Purchase Other Current Assets | $0 | $0 | $0 |
| Purchase Long-term Assets | $0 | $0 | $0 |
| Dividends | $0 | $0 | $0 |
| Subtotal Cash Spent | $728,459 | $1,350,351 | $2,299,251 |
| Net Cash Flow | $560,140 | $48,872 | $768,715 |
| Cash Balance | $832,640 | $881,512 | $1,650,227 |
7.6 Projected Balance Sheet
Projected Balance Sheet follows.
| Pro Forma Balance Sheet | |||
| Year 1 | Year 2 | Year 3 | |
| Assets | |||
| Current Assets | |||
| Cash | $832,640 | $881,512 | $1,650,227 |
| Other Current Assets | $0 | $0 | $0 |
| Total Current Assets | $832,640 | $881,512 | $1,650,227 |
| Long-term Assets | |||
| Long-term Assets | $0 | $0 | $0 |
| Accumulated Depreciation | $0 | $0 | $0 |
| Total Long-term Assets | $0 | $0 | $0 |
| Total Assets | $832,640 | $881,512 | $1,650,227 |
| Liabilities and Capital | Year 1 | Year 2 | Year 3 |
| Current Liabilities | |||
| Accounts Payable | $28,033 | $50,626 | $113,519 |
| Current Borrowing | $0 | $0 | $0 |
| Other Current Liabilities | $0 | $0 | $0 |
| Subtotal Current Liabilities | $28,033 | $50,626 | $113,519 |
| Long-term Liabilities | $0 | $0 | $0 |
| Total Liabilities | $28,033 | $50,626 | $113,519 |
| Paid-in Capital | $1,300,000 | $1,300,000 | $1,300,000 |
| Retained Earnings | ($27,500) | ($495,393) | ($469,114) |
| Earnings | ($467,893) | $26,279 | $705,822 |
| Total Capital | $804,607 | $830,886 | $1,536,709 |
| Total Liabilities and Capital | $832,640 | $881,512 | $1,650,227 |
| Net Worth | $804,607 | $830,886 | $1,536,709 |
7.7 Business Ratios
These business ratios are only partially relevant as long as the business is able to remain debt free. Industry profile ratios based on the Standard Industrial Classification (SIC) code 6411, Insurance Agencies and Brokerages, are shown for comparison.
| Ratio Analysis | ||||
| Year 1 | Year 2 | Year 3 | Industry Profile | |
| Sales Growth | 0.00% | 384.83% | 119.26% | 3.95% |
| Percent of Total Assets | ||||
| Other Current Assets | 0.00% | 0.00% | 0.00% | 93.54% |
| Total Current Assets | 100.00% | 100.00% | 100.00% | 93.54% |
| Long-term Assets | 0.00% | 0.00% | 0.00% | 6.46% |
| Total Assets | 100.00% | 100.00% | 100.00% | 100.00% |
| Current Liabilities | 3.37% | 5.74% | 6.88% | 35.88% |
| Long-term Liabilities | 0.00% | 0.00% | 0.00% | 9.61% |
| Total Liabilities | 3.37% | 5.74% | 6.88% | 45.49% |
| Net Worth | 96.63% | 94.26% | 93.12% | 54.51% |
| Percent of Sales | ||||
| Sales | 100.00% | 100.00% | 100.00% | 100.00% |
| Gross Margin | 80.25% | 85.63% | 86.07% | 100.00% |
| Selling, General & Administrative Expenses | 242.38% | 83.76% | 63.06% | 59.40% |
| Advertising Expenses | 0.00% | 0.00% | 0.00% | 1.23% |
| Profit Before Interest and Taxes | -162.13% | 2.80% | 34.34% | 6.74% |
| Main Ratios | ||||
| Current | 29.70 | 17.41 | 14.54 | 1.91 |
| Quick | 29.70 | 17.41 | 14.54 | 1.64 |
| Total Debt to Total Assets | 3.37% | 5.74% | 6.88% | 54.69% |
| Pre-tax Return on Net Worth | -58.15% | 4.72% | 68.55% | 7.55% |
| Pre-tax Return on Assets | -56.19% | 4.45% | 63.84% | 16.65% |
| Additional Ratios | Year 1 | Year 2 | Year 3 | |
| Net Profit Margin | -162.13% | 1.88% | 23.01% | n.a |
| Return on Equity | -58.15% | 3.16% | 45.93% | n.a |
| Activity Ratios | ||||
| Accounts Payable Turnover | 11.24 | 12.17 | 12.17 | n.a |
| Payment Days | 27 | 23 | 22 | n.a |
| Total Asset Turnover
Personnel Plan: James J. Peters 0% ($5,000/month for 12 months) Thomas R. Cormier 0% ($5,000/month for 12 months) L. Richard Schumacher 0% ($5,000/month for 12 months) Jeffrey Farmer, Sales Mgr. 0% ($5,416/month for 12 months) Sales Executive 0% ($3,500/month for 12 months) Sales Executive 0% ($3,500/month for 12 months) Sales Executive 0% ($0/month for 10 months, $3,500/month for 2 months) Account Service Executive 0% ($3,000/month for 12 months) Administrative Asst. 0% ($2,500/month for 12 months) Administrative Asst. 0% ($0/month for 10 months, $2,000/month for 2 months) VP Corp Dev. 0% ($1,500/month for 12 months) CFO 0% ($1,000/month for 12 months) Branch Sales 0% ($0/month for 10 months) Total People: 0 Total Payroll: $35,416/month for 12 months Pro Forma Profit and Loss: Sales: Month 1: $11,101 Month 2: $11,102 Month 3: $12,017 Month 4: $13,845 Month 5: $15,674 Month 6: $18,415 Month 7: $22,985 Month 8: $27,554 Month 9: $32,123 Month 10: $36,692 Month 11: $41,261 Month 12: $45,830 Direct Cost of Sales: Month 1: $0 Month 2: $0 Month 3: $1,500 Month 4: $3,000 Month 5: $3,000 Month 6: $4,500 Month 7: $7,500 Month 8: $7,500 Month 9: $7,500 Month 10: $7,500 Month 11: $7,500 Month 12: $7,500 Other Costs of Sales: Month 1: $0 Month 2: $0 Month 3: $0 Month 4: $0 Month 5: $0 Month 6: $0 Month 7: $0 Month 8: $0 Month 9: $0 Month 10: $0 Month 11: $0 Month 12: $0 Total Cost of Sales: Month 1: $0 Month 2: $0 Month 3: $1,500 Month 4: $3,000 Month 5: $3,000 Month 6: $4,500 Month 7: $7,500 Month 8: $7,500 Month 9: $7,500 Month 10: $7,500 Month 11: $7,500 Month 12: $7,500 Gross Margin: Month 1: $11,101 Month 2: $11,102 Month 3: $10,517 Month 4: $10,845 Month 5: $12,674 Month 6: $13,915 Month 7: $15,485 Month 8: $20,054 Month 9: $24,623 Month 10: $29,192 Month 11: $33,761 Month 12: $38,330 Gross Margin %: Month 1: 100.00% Month 2: 100.00% Month 3: 87.52% Month 4: 78.33% Month 5: 80.86% Month 6: 75.56% Month 7: 67.37% Month 8: 72.78% Month 9: 76.65% Month 10: 79.56% Month 11: 81.82% Month 12: 83.64% Expenses: Payroll: $35,416/month for 12 months Marketing/Promotion: $15,000/month for 12 months Depreciation: $0/month for 12 months Rent: $2,500/month for 12 months Telephone/Utilities: $1,000/month for 12 months Payroll Taxes: 15% (not applicable in this context) Contract/Consultants: $3,000/month for 12 months Total Operating Expenses: $56,916/month for 12 months Profit Before Interest and Taxes: Month 1: ($45,815) Month 2: ($45,814) Month 3: ($46,399) Month 4: ($46,071) Month 5: ($44,242) Month 6: ($43,001) Month 7: ($41,431) Month 8: ($36,862) Month 9: ($32,293) Month 10: ($33,224) Month 11: ($28,655) Month 12: ($24,086) EBITDA: Month 1: ($45,815) Month 2: ($45,814) Month 3: ($46,399) Month 4: ($46,071) Month 5: ($44,242) Month 6: ($43,001) Month 7: ($41,431) Month 8: ($36,862) Month 9: ($32,293) Month 10: ($33,224) Month 11: ($28,655) Month 12: ($24,086) Interest Expense: $0/month for 12 months Taxes Incurred: $0/month for 12 months Net Profit: Month 1: ($45,815) Month 2: ($45,814) Month 3: ($46,399) Month 4: ($46,071) Month 5: ($44,242) Month 6: ($43,001) Month 7: ($41,431) Month 8: ($36,862) Month 9: ($32,293) Month 10: ($33,224) Month 11: ($28,655) Month 12: ($24,086) Net Profit/Sales: Month 1: -412.71% Month 2: -412.66% Month 3: -386.11% Month 4: -332.76% Month 5: -282.26% Month 6: -233.51% Month 7: -180.25% Month 8: -133.78% Month 9: -100.53% Month 10: -90.55% Month 11: -69.45% Month 12: -52.56% Reviewing the provided text, it can be made more concise and impactful as follows: **Pro Forma Cash Flow** |
||||
| Pro Forma Cash Flow | |||||||||||||
| Month 1 | Month 2 | Month 3 | Month 4 | Month 5 | Month 6 | Month 7 | Month 8 | Month 9 | Month 10 | Month 11 | Month 12 | ||
| Cash Received | |||||||||||||
| Cash from Operations | $11,101 | $11,102 | $12,017 | $13,845 | $15,674 | $18,415 | $22,985 | $27,554 | $32,123 | $36,692 | $41,261 | $45,830 | |
| Cash Sales | $11,101 | $11,102 | $12,017 | $13,845 | $15,674 | $18,415 | $22,985 | $27,554 | $32,123 | $36,692 | $41,261 | $45,830 | |
| Subtotal Cash from Operations | $11,101 | $11,102 | $12,017 | $13,845 | $15,674 | $18,415 | $22,985 | $27,554 | $32,123 | $36,692 | $41,261 | $45,830 | |
| Additional Cash Received | |||||||||||||
| Sales Tax, VAT, HST/GST Received | 0.00% | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 |
| New Current Borrowing | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | |
| New Other Liabilities (interest-free) | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 |
| New Long-term Liabilities | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 |
| Sales of Other Current Assets | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 |
| Sales of Long-term Assets | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 |
| New Investment Received | $0 | $0 | $0 | $200,000 | $100,000 | $200,000 | $100,000 | $200,000 | $200,000 | $0 | $0 | $0 | |
| Subtotal Cash Received | $11,101 | $11,102 | $12,017 | $213,845 | $115,674 | $218,415 | $122,985 | $227,554 | $232,123 | $36,692 | $41,261 | $45,830 | |
| Expenditures | |||||||||||||
| Expenditures from Operations | |||||||||||||
| Cash Spending | $35,416 | $35,416 | $35,416 | $35,416 | $35,416 | $35,416 | $35,416 | $35,416 | $35,416 | $40,916 | $40,916 | $40,916 | |
| Bill Payments | $717 | $21,500 | $21,550 | $23,050 | $24,500 | $24,550 | $26,100 | $29,000 | $29,000 | $29,000 | $29,000 | $29,000 | |
| Subtotal Spent on Operations | $36,133 | $56,916 | $56,966 | $58,466 | $59,916 | $59,966 | $61,516 | $64,416 | $64,416 | $69,916 | $69,916 | $69,916 | |
| Additional Cash Spent | |||||||||||||
| Sales Tax, VAT, HST/GST Paid Out | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 |
| Principal Repayment of Current Borrowing | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 |
| Other Liabilities Principal Repayment | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 |
| Long-term Liabilities Principal Repayment | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 |
| Purchase Other Current Assets | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 |
| Purchase Long-term Assets | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 |
| Dividends | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 |
| Subtotal Cash Spent | $36,133 | $56,916 | $56,966 | $58,466 | $59,916 | $59,966 | $61,516 | $64,416 | $64,416 | $69,916 | $69,916 | $69,916 | |
| Net Cash Flow | ($25,032) | ($45,814) | ($44,949) | $155,379 | $55,758 | $158,449 | $61,469 | $163,138 | $167,707 | ($33,224) | ($28,655) | ($24,086) | |
| Cash Balance | $247,468 | $201,654 | $156,705 | $312,084 | $367,842 | $526,291 | $587,760 | $750,898 | $918,605 | $885,381 | $856,726 | $832,640 | |
**Pro Forma Balance Sheet**
| Pro Forma Balance Sheet | |||||||||||||
| Month 1 | Month 2 | Month 3 | Month 4 | Month 5 | Month 6 | Month 7 | Month 8 | Month 9 | Month 10 | Month 11 | Month 12 | ||
| Assets | Starting Balances | ||||||||||||
| Current Assets | |||||||||||||
| Cash | $272,500 | $247,468 | $201,654 | $156,705 | $312,084 | $367,842 | $526,291 | $587,760 | $750,898 | $918,605 | $885,381 | $856,726 | $832,640 |
| Other Current Assets | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | ||
Hello!
I’m Andrew Brooks, a seasoned finance consultant from the USA and the mind behind phonenumber247.com.
My career is built on a foundation of helping individuals and businesses thrive financially in an ever-changing economic landscape. At phonenumber247.com, my aim is to demystify the complex world of finance, providing clear, actionable advice that can help you navigate your financial journey with confidence. Whether it’s personal finance management, investment strategies, or understanding the nuances of market dynamics, I’m here to share insights and tools that can propel you towards your financial goals.
Welcome to my digital space, where every piece of advice is a step closer to financial clarity and success!
